Note from the Author: This
information was written with inspirations taken from Allergy Clinic Veterans, Nurse
Executive Director - Marilyn Crosby, Nurse Managers - Althea Phillips-Edwards,
Monike Harvey, Sy Reeker, Prime Care Clinic Director - Dr. Nicholas Masozera, Allergy
Clinic Doctors - Dr. Roger Rossen (initiator), Dr. Frank Orson, Dr. David Corry
and Dr. Adrian Casillas, Allergy Clinic Staff Registered Nurses –Alberta E. Gudes
(writer), Jodi Francis, Estelita Mansukhani, and Nathasha Mingo-Foster and all
Prime Care Clinic Staff at Michael E. DeBakey Veterans Affairs Medical Center and
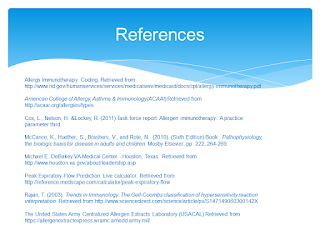
Excerpts from Kathryn L. McCance, Sue E.
Huether, Valentina L. Brashers and Neal S. Rote. 2010. (Sixth Edition) Book: Pathophysiology, the biologic basis for
disease in adults and children. Mosby Elsevier. pp. 222, 264-269.
Allergy
Allergy is a
hypersensivity response against an environmental antigen (allergen). The most
common allergies are type I hypersensitivities, although any of the other three
mechanisms may cause allergic responses.
Veterans had similar experiences of the common allergens.
Typical allergens that
induce type I hypersensitivity include pollens (e.g. ragweed), molds and fungi
(e.g. Penicillum notatum), foods
(e.g. milk, eggs, and fish), animals (e.g. cat dander, dog dander), cigarette
smoke, components of house dust (e.g. fecal pellets of house mites) and almost
anything else we may encounter in our environment. Allergens that primarily
elicit type IV allergic hypersensitivity include plant resins (e.g. poison ivy,
poison oak), metals (e.g. nickel, chromium), acetylates and chemicals in
rubber, cosmetic, detergents and topical antibiotics (e.g. neomycin). Type II
and III allergic hypersensitivities are relatively rare but may include
antibiotics (e.g. penicillin, sulfonamides) and soluble antigens produces by
infectious agents (e.g. hepatitis B).
Usually a sensitization
process involving multiple exposures to the allergen occurs before adequate
amounts of antibody or T cells are available to elicit a hypersensitivity
response. In some instances, exposure to a particular allergen may not be
apparent in the case of allergens that are drugs, additives, or preservatives
in food. For example, milk may contain trace of amounts of penicillin used for
treating cows for mastitis. Thus, the first therapeutic exposure to penicillin
may cause unexpected hypersensitivity reaction. Additionally, penicillin shares
a B-lactam structure with
cephalosporin, so that one antibiotic may be sensitive against another.
Genetic Predisposition
Certain individual are
genetically predisposed to develop allergies, particularly type I allergies,
and are called atopic. In families in
which one parent has an allergy, allergies develop in about 40% of the
offspring. If with both parents have allergies, the incidence in the offspring
maybe as high as 80% according to Principles of Genetics.
Atopic individuals tend to produce higher quantities
of IgE (immunoglobulins) and to have more Fc (crystalline fragment) receptors
for IgE on their mast cells. The airways and the skin of atopic individuals are
also more responsive to a wide variety of both specific and nonspecific stimuli
than are the airways and individuals who are not atopic. Multiple genes have
been associated with the atopic state, including polymorphism in a large
variety of cytokines that regulates IgE synthesis (e.g. interleukin and
cellular receptors.
Clinical Symptoms of
Type I Allergies
The clinical
manifestations of type I reactions are attributable mostly to the biologic
effects of histamine. Tissues most
commonly affected contain large numbers of mast cells and are sensitive to the
histamine released from them. These tissues are found in the gastrointestinal
tract, the skin, and the respiratory tract. The particular symptoms reflect the
main portal of entry for the allergen. For instance, pollens are airborne
allergens usually cause respiratory symptoms.
Effects of allergen on
the mucosa of the eyes, nose, and respiratory tract include conjunctivitis
(inflammation of the membranes lining the eyelids), rhinitis (inflammation of
the mucous of the membranes of the nose), and asthma (constriction of the
bronchi). Symptoms are caused by
vasodilation, hypersecretion of mucus, edema, and swelling of the respiratory
mucosa. Because the mucous membranes lining the respiratory tract (accessory)
sinuses, nasopharynx, and upper and lower respiratory tract are continuous,
they are all adversely affected. The degree to which each is affected determines
the symptoms of the disease.
Gastrointestinal
allergies are caused primarily by allergens that enter through the mouth –
usually foods or medicines. Symptoms include vomiting, diarrhea, or abdominal
pain and may be severe enough to result in malabsorption or protein-losing
enteropathy, if the reactions are prolonged or recurrent. Foods most often
implicated in gastrointestinal allergies are milk, chocolate, citrus fruits,
eggs, wheat, nuts, peanut butter, and fish. When food is the allergen, the
active immunogen may be a product of food breakdown by digestive enzymes.
Urticaria or hives, is a dermal
(skin) manifestation of type I allergic reactions. The underlying mechanism is
the localized release of histamine and increase vascular permeability,
resulting in limited areas of edema. Urticaria is characterized by white fluid-filled
blisters (wheals) surrounded by areas of redness (flares). The wheal and flare reaction is usually accompanied by itching. Not all urticarial
symptoms are caused by allergic (immunologic) reactions. Some, termed nonimmunologic urticaria, result from
exposure to cold temperatures, emotional stress, medications, systemic
diseases, hyperthyroidism, or malignancies (e.g. lymphomas.)
If possible, avoidance of the allergen is the best method to
limit allergic responses. Approximately 30% of the laboratory animal handlers
have allergies to animal dander and must use face masks or other devices to
avoid contact.
Although some type I
allergic responses can be controlled by blocking histamine receptors with
antihistamines, the primary mechanism of control is the autonomic nervous
system. The autonomic nervous system includes biochemical mediators (e.g.
epinephrine, acetylcholine) that, like the mediators of the inflammatory
response, have profound effects on cells. These mediators bind to appropriate
receptors on mast cells and target cells of the inflammation (e.g. smooth
muscle) thereby controlling (1) release of inflammatory mediators from mast
cells and (2) the degree of which target cells respond to inflammatory
mediators.
Allergic Disease: Bee
Sting Allergy
An example of a
life-threatening allergy is an anaphylactic reaction to a bee sting. Bee venom contains
a mixture of enzymes and other proteins that may serve as allergens. About 1%
of veterans may have anaphylactic reaction to bee venom. Within minutes they
may develop excessive swelling (edema) at the bee sting site, followed by
generalized hives, itching, and swelling in areas distal from sting (e.g. eyes,
lips), and other systemic symptoms including flushing, sweating, dizziness, and
headache. The most severe symptoms may include gastrointestinal (e.g. stomach
cramps, vomiting), respiratory (e.g. tightness in the throat, wheezing,
difficulties breathing), and vascular (e.g. low blood pressure, shock)
reactions. Severe respiratory and vascular reactions may lead to death.
If a veteran has had a
previous anaphylactic response to bee stings, the chance of having another is
about 60%. During the reaction the
administration of antihistamines has a little effect because histamines has
already bound H1 receptors and initiated severe bronchial smooth muscle
contraction. Most individuals carry self-injectable epinephrine. Autonomic
nervous system mediators, such as epinephrine, bind to specific receptors on
smooth muscle and reverse the effects of histamine and result in muscle
relaxation. Similar anaphylactic reactions have been described against peanuts
and other nuts, shellfish, fish, milk, eggs, and some medications.
Test of IgE-Mediated
Allergy
Allergic reaction can be life threatening; therefore, it is
essential that severely allergic individuals be made aware of the specific
allergen against which they are sensitized and instructed to avoid contact with
that material. Several tests are available, including food challenges, skin
tests with allergens, and laboratory tests for total IgE and allergen-specific
IgE in the blood.
Reactivity to a
particular food allergen may be tested by controlled administration of small
doses of the suspected allergen in order to evoke a mild allergic response.
This approach can be dangerous if the individual has history of anaphylactic
responses. A safer approach is injection of an allergen into (intradermal) or onto
(epicutaneous or prick test) the skin. The individual is allergic to a
particular allergen, a local wheal and flare reaction within a few minutes at
the site of injection. The diameter of the flare reaction is usually indicative
of the individual’s degree of sensitivity to that allergen. In the most
severely allergic individuals even the extremely small amounts of allergen used
for the skin tests may evoke a systemic anaphylaxis. Skin test is also
contraindicated if the patient is using medications that may affect the test or
has diffuse dermatitis, which would make the reaction difficult to interpret.
Desensitization
(Immunotherapy)
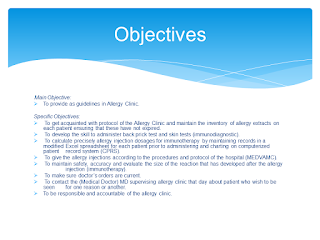
Clinical desensitization
to allergens can be achieved in some individuals. Minute quantities of the allergen are
injected in increasing doses over a prolonged period. The procedure may reduce
the severity of the allergic reaction in the treated individual. However, this
form of therapy is associated with a risk of systemic anaphylaxis, which can be
severe and life threatening. This approach works best for allergies against
some food allergens and with biting insect allergies (80% to 90% rate of
desensitization over 5 years of treatment.
The mechanism by which
desensitization occurs maybe several, one of which is the production of large
amounts of so-called blocking antibody,
usually circulating IgG. A blocking
antibody presumably competes in the tissues or in the circulation for
binding with antigenic determinants on the allergen so that the allergen is
“neutralized” and is unable to bind with IgE on mast cells. Desensitization
injections also may stimulate the generation of clones of regulatory T
lymphocytes, which inhibit hypersensitivity by suppressing the production of
IgE or modifying the Th1/Th2 interactions in favor of production of
anti-inflammatory cytokines.
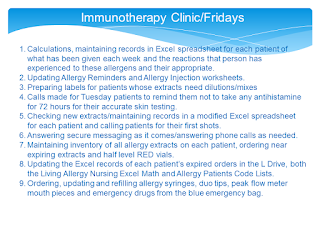
Benefits for Staff
The established knowledge above, benefits the Allergy Clinic
change from one day “Friday” 09:00-11:00 AM to three days “Monday, Wednesday,
and Thursdays from 08:00 to 10:00 AM:
(1) Allergy staff nurses can attend the Prime Care
Staff meeting from 08:00 to 09:00 AM on Fridays which appropriately can include
a robust sense of communication and collegiality of the Prime Care Clinic and
updates nursing management challenges and changes from the Nursing Management
view.
(2) Allergy clinic veterans expected and provided
with exclusive allergy nursing skills that another may not possess e.g.
veterans has other day’s options to take allergy injections.
(3) Allergy team members feel that very high
quality patient care is delivered with safe and supportive environment.
(4) It is very rewarding to see challenging
high-risk allergy clinic patients become better self-managers, teachers and
motivators for other patients, and have improved health outcome.
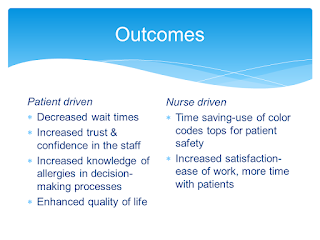
Benefits for Veterans
(1) Veterans may benefit from the one-on-one visit
access to multiple disciplines or areas of expertise (allergy disease
medication management, nutrition, and behavioral/motivation experts e.g.
smoking cessation counseling) while taking allergy injections or immunotherapy.
(2) Patients also benefit from the experience of
other patients participating in the group allergy clinic (peer support) with
allergy staff guidance, patients learn from each other about solutions to
tackle the day-to-day challenges in a way that is impossible to achieve in
traditional clinic visits.
(3) Finally, the patients gain commitment, a sense
of control; usually voiced experience improved health, and need to come to
allergy clinic weekly even the every other weekly maintenance dosing was reached.